COVID19 Resources
Wellness
Documents
- CDC — How to Self-Quarantine
- ODH COVID Testing Algorithm
(updated version 3/13/29) This algorithm isn’t perfect, but it’s pretty good. It’s the most recent thing provided by ODH. ODH isn’t necessarily the same as LDH and they’re not always on the same page, but at least it’s something to help guide you in a complex, ever-changing situation.
Media
- Calhoun Grand Round COVID19 Update
NOTE: Changes since talk given on 3/4/20- Reuse of N95s is not applicable to COVID-19 due to the contact precautions portion of the disease. Only applies to TB.
- The definition of PUI had significantly changed since this lecture. Please see cdc.gov for current definition (much more broad)
- Current UCMC cohorting plan involved 7 NW, not Ridgeway
Announcements and Communications
EM COVID19
We are going to open the RESPIRATORY ED tomorrow (in almost all certainty). Here is how things will go down, KEEPING IN MIND that things WILL change, perhaps frequently, depending on what this looks like. Planning for continued escalation is ongoing. I very much appreciate your patience in the coming days, and the strain that we are about to put on our staff to accomplish this herculean lift.
- SCREENING TENT: Patients will be screened at the front door and if they screen positive for ANY respiratory complaint, they will be sent to the RESPIRATORY ED, which will start as a TENT outside of the decon room in the parking lot where A-Pavillion used to stand, where 2 trees stand now, and our future ED will stand.
- SCREENING: Patients for now will be screened by a NURSE in the tent, which will serve as a Waiting room/screening area. The tent is heated, has electric, will have masks, PPE, etc. We are working on Wi-FI in the tent, and it will have Portable Toilets outside. It should have a sink for hand washing, I believe. Security WILL be present in the tent.
- This tent will LIKELY turn into a MD/APP driven screening area when volumes dictate. We need to prep a bit more on how to staff this with another “extra” provider.
- CDU ADMISSION: Patients will be sent into the CDU via the south hallway, which will be closed to general traffic. An attending and a nurse will be stationed in rooms 1-5 in appropriate PPE where we will perform Medical Screening Exams on patients. There, we will determine do you need testing, do you need to be in the hospital, or can you get out of this department ASAP. Consider the following:
- All you probably need to make a solid decision is an O2 sat, what day of illness they are on (most getting SICK past 1 week), and what are their co-morbidities. Particularly, lung disease (asthma, COPD, ILD), immune suppression, bad diabetic, older (>65), you know the drill. If it gets bad enough, prepare to loosen your standards of those co-morbidities based on what the patient looks like right now in front of you, not what they might look like tomorrow. We aren’t there….yet.
- EVS is going to be an issue in this screening area. We will likely need to shoulder a significant cleaning burden. If there is no EVS available, please wipe down chairs/tables with blue top (bleach) wipes after each encounter, and wait 3 minutes for it to dry before bringing in the next patient.
- All you probably need to make a solid decision is an O2 sat, what day of illness they are on (most getting SICK past 1 week), and what are their co-morbidities. Particularly, lung disease (asthma, COPD, ILD), immune suppression, bad diabetic, older (>65), you know the drill. If it gets bad enough, prepare to loosen your standards of those co-morbidities based on what the patient looks like right now in front of you, not what they might look like tomorrow. We aren’t there….yet.
- TESTING: Emergency Management has loosened the standards for the ED regarding calling 584-WASH, given its lack of efficiency. We are the only group thus far to get that, and thanks to Dustin Calhoun for allowing this to happen.
- Guidelines on WHO to test:
- ANYONE who is getting admitted
- ANYONE who has been in contact with a COVID-19 positive patient in the last 2 weeks
- ANYONE who ODH sends in to be tested (more on this below)
- ANYONE who you think in your CLINICAL judgement should be tested, i.e.- just got off a flight from Seattle with symptoms, just came from China, etc. This is now under your discretion. Please remember, testing is limited, so be prudent.
- Guidelines on HOW to test:
- Right now (this WILL change), our main testing platform is through LabCorp. In order to test for this, order in EPIC using test code LAB4674, 2019 Novel Coronavirus (Covid-19), NAA. This will trigger send out of the sample to LabCorp
- For testing to be sent to the Ohio Department of Health (following ODH request), do not use the EPIC test code above. Instead, continue to order a miscellaneous test (AREF) in EPIC and add the comment “ODH Covid-19—do not send to LabCorp”.
- Swabs to be used for COVID19 testing cannot also be used for other microbiology studies. If other tests are needed in addition to the COVID-19 test, please send a separate swab for each test.
- Remember- doing an NP swab requires Airborne + Droplet + Contact precautions (full monte)
- Guidelines on HOW to TRACK:
- If you want to test, please call 584-WASH, select option 1 (voice recording) and leave the name, medical record number, and if they were an ODH test or LabCorp test. That’s all we have to do now. Then they will track the tests on the back end.
- Guidelines on WHO to test:
- Workup/Admission: If a patient needs to be worked up/admitted (hypoxia, concerning co-morbidities, looks sick, etc.), move them to a room in CDU 6-16. There, an APP +/- resident can begin a full workup.
- Workup for now should include: CBC, Renal, LFTs, INR, CRP, blood cultures, Influenza swab, +/- Respiratory panel (still confirming if Infection control wants this), CXR, +/- non-con CT chest
- Admit to either medicine or MICU based on severity of illness. Admit them QUICKLY. Try not to hem and haw, if they are sick, admit them (particularly for elderly, hypoxic, immunosuppressed, or lung disease patients). The goal of screening is to only get sick patients to the rooms anyways.
- We have (some) assurances that these patients will be moved up quickly.
- Intubations/patient management in the CDU:
- If a patient is sick enough to need to be intubated in the CDU, we must follow Airborne precautions and donning/doffing recommendations based on institutional guidelines as well as outlined by Dr. Carleton in the most recent I.C.Cordes email. If there are residents (R4/R1) in the Respiratory ED, the R4 will be the only resident that can intubate currently. The Attending will be back up. If there are no residents, the attendings will intubate.
- DO NOT use NIPPV (CPAP/BILevel) on these patients, attempt to use Hi-Flo NC at MOST.
- Start with regular NC up to 4-6L, transition to HFNC, and if you continuing to increase HFNC without improvement- INTUBATE the patient.
- AVOID nebulized treatments in almost all these patients except the bad asthmatics or bad COPD patient
- AVOID steroids in most of these patients except the severe asthma/COPD patient
- AVOID empiric antibiotics if your clinical suspicion is related to COVID-19 viral infection/pneumonia- draw cultures and let the team follow
- AVOID IV FLUIDS in most of these patients who have no hemodynamic instability- most of these patients are NOT “septic” or in shock on presentation. Excess fluid administration dramatically worsens patients who progress to ARDS (common in these sicker patients)
- OB patients
- The health system has requested (appropriately) for us to assist in keeping potential COVID-19 patients out of the maternity NICU areas if possible. Here is what we have devised:
- Because of the health concern, all OB patients (including >16 weeks) with respiratory complaints will come through the Respiratory ED. Screen them the same way you would a normal patient- healthy moms don’t need to be there AND only need to be tested if admitted.
- If the patient appears sick or has lung pathology (asthma), move them to a room, work them up (standard) and call OB- they will come to the bedside, and work to expedite that patient upstairs to the 7th floor (MSD or MICU)
- If the patient appears sick or has lung pathology (asthma), move them to a room, work them up (standard) and call OB- they will come to the bedside, and work to expedite that patient upstairs to the 7th floor (MSD or MICU)
- Patients who show up to the ED but do not have respiratory complaints will still be sent up to the 3rd floor per our usual practice
- Laboring mothers who have concern for COVID should be masked immediately and sent upstairs to the saved negative pressure room on the 3rd floor in the OBED. The ED charge RN will alert the OB Charge RN
- Staffing of the Respiratory ED
- Attending coverage:
- UHS1 becomes 0700-1900 and staffs the Respiratory ED. Responsibilities are to be primary screener and supervise APP (+/- resident) in rooms 6-16
- UHS2 becomes 1900-0700 and staffs the Respiratory ED.
- UHA/B and UH1/2/3 to cover Minor Care supervision
- ***NOTE*** Anticipated change we are NOT yet doing (I will let you know)- if volumes increase dramatically, we will convert the UH2 to a 10-12-hour screening shift in the tent to allow the S1/S2 to manage multiple sicker patients in the back with the APP. The shift times will likely be in the 10-11am range until 8-11pm range. More to come!
- APP coverage:
- U1: Shift will move to 0700-1900 and will work in the Respiratory ED
- OBS1: Maintains ED Observation patient care in the Main ED
- OBS2: Will work the overnight shift in the Respiratory ED
- Resident Coverage:
- Staffing will depend on the volume of the Main ED. Huddles should occur at 0700 and 1900. If boarding is such that B/Cpod are closed, the R1/R4s can work in the Respiratory ED to see patients. We must have at least one extra resident to in Dpod to staff the V4-V9 beds vacated by the U1 APP. If for some reason there are multiple open beds in B/C pod, the R4/R1 team can stay in the Main ED. Shift dependent process with built in flexibility.
- Attending coverage:
Attendings: I know this is nuts. We are asking so much, and for that, I apologize and am profoundly thankful. We have looked at the next 2 weeks thus far, and found only 2 people who have conflicting shift obligations the next day after a move from the normal S2 to a night shift S2. We will work on that individually.
- We will be asking for volunteers to cover shifts that we can anticipate cannot be filled (example- no shift to steal to cover weekend Respiratory ED nights, thus, need volunteers).
- We may ask you to do things that are uncomfortable- rapid medical screening exams, moving to different care areas, etc., that vary day to day, or hour to hour. This is unprecedented and we aren’t sure how its going to go down, but we have the right people in this EM group to make it work and get each others backs.
9) Respiratory ED OPS stuff:
- We have tried to think of everything to open an entirely new ED in less than a week, but we will miss things. PLEASE let me know what works in this unit, and what doesn’t. But please, try to just let me know the big stuff. This will not be perfect, in fact, far from it. But if it's functional and serves its purpose to cohort COVID, minimize staff impact, improve screening and flow, and do it as safely as possible, then it will be a win.
- For awareness, we are ensuring we have security, registration, RT, pharmacy, lab, rads, food services, EVS, transportation, etc. all have processes to be up and running ASAP in this unit.
That is all I have for tonight. More to come in the next few days- I will review what has gone well and what hasn’t. Be ready for emails requesting for volunteer coverage for shifts to be paid at our OT rate, starting already for this weekend Saturday and Sunday night in the Respiratory ED.
Hopefully some of you were privy to Sanjay’s amazing email to his WCH team, including this excerpt that was particularly incredible-
“But MOST IMPORTANTLY, what I want you to know is that there is no other department I’d rather face this with. We’re going to get hit by this impending storm, but we’re going to face it together. And we will get through this. Times will get hard, and every person in our family will need a pick-me-up here and there- I know I will. I have always felt we had the coolest job in the world. It's now become one of the most important jobs in the world. While everyone else is ordered to stay home, we’re asked to come in, and that’s for a reason. Because we’re needed to make a difference. And we will”
Outstanding. THIS is why we went into Emergency Medicine, right? EVERYONE is looking at us right now- let’s stand up and show ‘em why we are the best damn department in the country.
Thanks,
Jack
Jack P. Palmer III, M.D., M.S.
Provided by Calhoun 3/10/20
Criteria to Guide Evaluation and Laboratory Testing for COVID-19
Clinicians should work with their local and state health departments to coordinate testing through public health laboratories. In addition, COVID-19 diagnostic testing, authorized by the Food and Drug Administration under an Emergency Use Authorization (EUA), is becoming available in clinical laboratories. This additional testing capacity will allow clinicians to consider COVID-19 testing for a wider group of symptomatic patients.
Clinicians should use their judgment to determine if a patient has signs and symptoms compatible with COVID-19 and whether the patient should be tested. Most patients with confirmed COVID-19 have developed fever1 and/or symptoms of acute respiratory illness (e.g., cough, difficulty breathing). Priorities for testing may include:
- Hospitalized patients who have signs and symptoms compatible with COVID-19 in order to inform decisions related to infection control.
- Other symptomatic individuals such as, older adults (age ≥ 65 years) and individuals with chronic medical conditions and/or an immunocompromised state that may put them at higher risk for poor outcomes (e.g., diabetes, heart disease, receiving immunosuppressive medications, chronic lung disease, chronic kidney disease).
- Any persons including healthcare personnel , who within 14 days of symptom onset had close contact with a suspect or laboratory-confirmed COVID-19 patient, or who have a history of travel from affected geographic areas (see below) within 14 days of their symptom onset
There are epidemiologic factors that may also help guide decisions about COVID-19 testing. Documented COVID-19 infections in a jurisdiction and known community transmission may contribute to an epidemiologic risk assessment to inform testing decisions. Clinicians are strongly encouraged to test for other causes of respiratory illness (e.g., influenza).
Mildly ill patients should be encouraged to stay home and contact their healthcare provider by phone for guidance about clinical management. Patients who have severe symptoms, such as difficulty breathing, should seek care immediately. Older patients and individuals who have underlying medical conditions or are immunocompromised should contact their physician early in the course of even mild illness.
Colleagues,
Updates from the last 24 hours. Continually honored to work with this team who selflessly do whatever is asked without hesitation, even if it changes hour to hour. Protocol changes, shift changes, shift pick-ups, extra work, you name it, EVERYONE is pitching in. It’s awesome.
1) The Respiratory ED ribbon cutting was yesterday at 3pm, performed by Dr. Conal Roche. By all accounts, he was the perfect person to kick us off, as you'd expect. Thank you to Conal for his great attitude, flexibility, and great ideas as we got started.
2) Saw a good number of patients through the Respiratory ED. Note the following protocols and lessons learned:
- We are seeing ANY respiratory complaint back there, and likely most febrile illnesses. GI bleed with a cough, abdominal pain with shortness of breath were fair game.
- We are NOT moving these patients back to the Main ED if we think they are low risk for COVID-19. Anticipating that soon, few will be considered low risk. Patients who may end up being respiratory patients CAN be moved to the Respiratory ED.
- Patients are being escorted from the tent (waiting room/first triage/registration) to rooms 1-5 for screening. If sicker or need workup- send to room 6-16, if well, discharge.
- Attending and APP basically just split up patients all shift, no real need based on volume for one "screener". May have to change that soon, though.
- No intubations or sick COVID-19s up until this AM. Saw a few potentials that were swabbed and discharged (more on that later)
- If you get someone who is VERY sick back here, please consider calling for help, or if necessary moving to the SRU (last resort).
- Got Dragon installed on a second computer in the Nursing station
- NO PPE in the Nursing station- must be doffed prior to entry
2) Please see the new attached testing algorithm. Much clearer, and thanks to Dustin for advocating for us to make this clear and as simple as they would allow, and Sanjay for laying it all out. STRONG WORK. We did this over the past 18 hours in the Respiratory ED and it is smooth. ODH was helpful the few ODH cases we did, and for the rest that were more “clinical judgement” testing, LabCorp was easy.
3) Thanks to Lisa Kiser for getting that discharge dot phrase together. You can add yourself to it by going to “My Smartphrases”, searching “Kiser, L”, and finding her .lwcovid discharge phrase, which is based off of the CDC recs for testing suspected patients who can/should go home and self quarantine. We are also telling patients to register and log into MyChart where they can follow up their results, and LabCorp SHOULD be calling (but have them logon just in case).
4) BIG MISS from JP: I failed to mention in our new staffing model- because the OBS2 APP is covering in the Respiratory ED from 7p-7a, overnight the POD docs will managed ED CDU OBS Protocols that exist in their care space, and if not, from where they originated. The Attendings are already “aware” of the protocol patients that they own, but now the care team in their space truly owns their care- pain control, lab/imaging follow up, etc. The OBS1 APP will find the appropriate attending and inform them around signout the final plan, and the Attendings and residents must manage these patients to the best of their abilities overnight. Ultimately, not much happens with OBS patients overnight, but often times results are completed, sometimes patients are discharged, and often admitted overnight. The OBS2 can help with operational issues (showing how to admit, how to order something, figure out if we can get a DVT study, etc.), but they are committed to the Respiratory ED and will NOT be caring for these patients for the foreseeable future.
5) A new OBS clarification- due to the high concern of asthmatics and COPD patients to potentially have COVID-19 and possibly decompensate rapidly, we will NOT be admitting any Asthma/COPD patients to ED OBS Protocols until we have a better control over this disease process. From my readings, these patients are getting incredibly sick, but the interval at which this occurs is hard to determine, and many rapidly decline over 8-12 hours and I do not want that falling on our Respiratory ED “keeping” these patients and managing them for 24 hours. Further, we may be falsely reassuring that a patient is “stable” for a day and ok to go, when they may crump shortly thereafter.
6) Last intubation update: Please officially clean the King Vision with a Blue Top Bleach wipe, which are on top of the intubation cart currently stationed in room 16. While that room is the largest and best for intubations, that cart is meant to be mobile from room to room. Keep the cart in the hallway and bring your clean supplies in with you when you don. Clean the King with the Blue top wipe after an intubation, place it in a clean biohazard bag (for now), doff your PPE, and bring the King out with you and replace it in the cart.
7) We are working to come up with the best strategy for asthma/COPD patients who need bronchodilators- nebs are a no-no unless they REALLY need them. Taking inventory of our MDI supply and may use more aggressive MDI protocols- more to come. Also, I mentioned the progression of O2 as NC to HFNC in my last email. Newer recs are stating that we should likely transition from NC to Face Mask (less aerosols) and if they aren’t doing well on NRB FM- intubate.
8) SCRUBS!!! There is a big bin outside of CPod doors next to the elevators in the Lab Building (like you are walking to the Men’s Locker room/CDU). PLEASE do yourself and your family a HUGE favor- wear clean clothes to work, change into scrubs, work, DOFF those scrubs, change into clothes and go home. Consider the same thing for shoes. It’s NOT WORTH IT. I know cargo pants are comfortable. I know black polos are back in style. Wear scrubs!
Thats all I’ve got for now, other than check out these pics! OPENING NIGHT AT THE RESPIRATORY ED!! Since everything else was closed, we decided to throw down.
Jack
1) PPE – please ensure that you are wearing appropriate PPE for ALL patients (regardless of severity) who present with a respiratory complaint. This means mask, gown, eye protection, and gloves.
a. Illness will mandate that employees stay out of work – that will be inevitable. However, losing docs and APPs that are otherwise asymptomatic but are quarantined due to inadequate PPE during patient contact will put even more of a strain on our system. I will be the first to admit that I was lax about doing this will all patients earlier in the week, and I apologize for setting a bad example
b. Regarding Masks – A surgical mask is all that is needed for most encounters (announced today am I told), with the EXCEPTION of more invasive airway procedures (bagging, intubating, bronching) which will require N95 (airborne precx)
c. If patients are super sick, they will stay in C pod if at all possible. Intubations, lines, everything can happen there.
2) Who to test – This is ever-evolving, and I welcome to Dustin to correct me if I’m wrong. Currently, we are testing for COVID on:
a. Patients being admitted with respiratory illness
b. >/= 65 year olds
c. Immunosuppressed (chemo or other meds)
d. Comorbid conditions – Obesity, Diabetes, heart disease, chronic kidney disease
e. Lung disease (asthma, COPD, ILD, etc)
f. Pregnant patients
g. Close contact with confirmed COVID-19 patient
h. Travel from Level 3 country (as of 3/13: Italy, China, South Korea, Iran)
Note that Flu and COVID can be sent from the same single swab. A respiratory viral panel requires an additional swab.
You can make this decision on your own for testing, or you can call 584-WASH for guidance.
3) WCH Triage Process - ***BRAND NEW*** The goal of this is to minimize exposure to our patients and our staff to the walking well. If we can safely avoid them entering the hospital doors, we will.
a. Arrival – patients who arrive by private vehicle will be greeted at the entrance by a medic. If they have fever, cough, shortness of breath, they will be given a mask. They will then be escorted to the big yellow tent that is now up outside.
i. If patients do not have COVID like symptoms, they will be taken to pods A or B
ii. If patients have COVID symptoms but have any of the factors in #2 above (need testing) OR if they have abnormal VS (HR>100, SBP<100, Sat <90) they will be taken to C pod
b. In the tent, they will be entered into EPIC by the nurse (via a WOW) and undergo a quick triage with vitals and basic info being taken.
1. Patients will be listed in “C-Hall” if they are in the tent.
c. They will then wait until a physician comes in to see them. This can be any attending, so please keep an eye on C-hall. If a patient has waited 2+ hours in the tent, or if >4 patients are in the tent, the charge nurse will call the 3377 phone
d. MSE – Patients will require a medical screening examination.
i. This is up to your comfort level and I don’t want you to feel unsafe, though it will be uncomfortable for many of us
ii. Please know that physical contact, including with a stethoscope, is NOT required for an MSE.
e. If the patient doesn’t seem well, let the nurse know and they will be taken to C pod for a more thorough workup
f. If the patient seems fit for discharge, please do a brief note (Jack and/or I will send out a template for a note in the next day or two), and then discharge them via EPIC with instructions to self-quarantine for 2 weeks (you can use Lisa’s .LWCOVIDDC smartphrase from the CDC – thank you for sharing, Lisa). They will be discharged home directly from the tent. (The nurse will print the discharge instructions)
4) Of note – the arrival process has not yet changed for EMS arrivals (Patients with respiratory complaints to C pod, all others to A and B pods)
Obviously fluid, and things will change. We’ll learn more as we continue and expand on this process. I welcome any and all feedback. Stay safe.
Sanjay
617-281-9416
Team,
Specific updates regarding workflow at WCH during the pandemic.
- The triage tent is up and running. Its purpose is to evaluate patients quickly, perform a medical screening exam, and potentially discharge patients without them ever entering the hospital.
- Testing cannot be done in the tent. Let the nurse know and they will be moved to C pod
- The patients that are well can be discharged from the tent (without testing)
- Remember a medical screening exam (MSE) does not require a stethoscope. The goal is to identify if an emergent condition is present or not. If not, you can send the patient home.
- We have developed triage sheets for the nurses to collect data – the triage nurse will input minimal data into EPIC (including PMH, etc). You can then use that sheet to dictate your note.
PLEASE DISCARD THE TRIAGE SHEET AFTER USE INTO A PHI PROTECTED BIN – IT IS NOT PART OF THE PERMANENT RECORD - Phones and workflow
- Call C pod rooms with 298-88## (## representing the room number of the patient).
- Nurses are to orient the patient to the phones and inform them that calls will be coming
- Hopefully you will only be in the rooms once (initial eval) for most patients
- Please also be mindful of the nurses’ exposure risk, and try to consolidate all of your orders as much as possible so they don’t have to make repeated trips into the rooms
- I understand over the weekend that one doctor was designated as the respiratory doc. I think that’s a brilliant idea. Feel free to continue this model. I’m the 3p-11p tomorrow so I’ll be interested to see how it works on the weekend
- I know the ODH calls have been a big pain. We are trying to devise ways to have ancillary staff perform those tasks, while Dustin keeps making pleas to decrease that at a state/county level. Thank you all for putting in that extra work.
Feedback, as always, is welcome.
Sanjay
Team,
Thank you for your continued flexibility as we work on improving processes in anticipation of what’s to come. A few EPIC updates for both Emergency Departments:
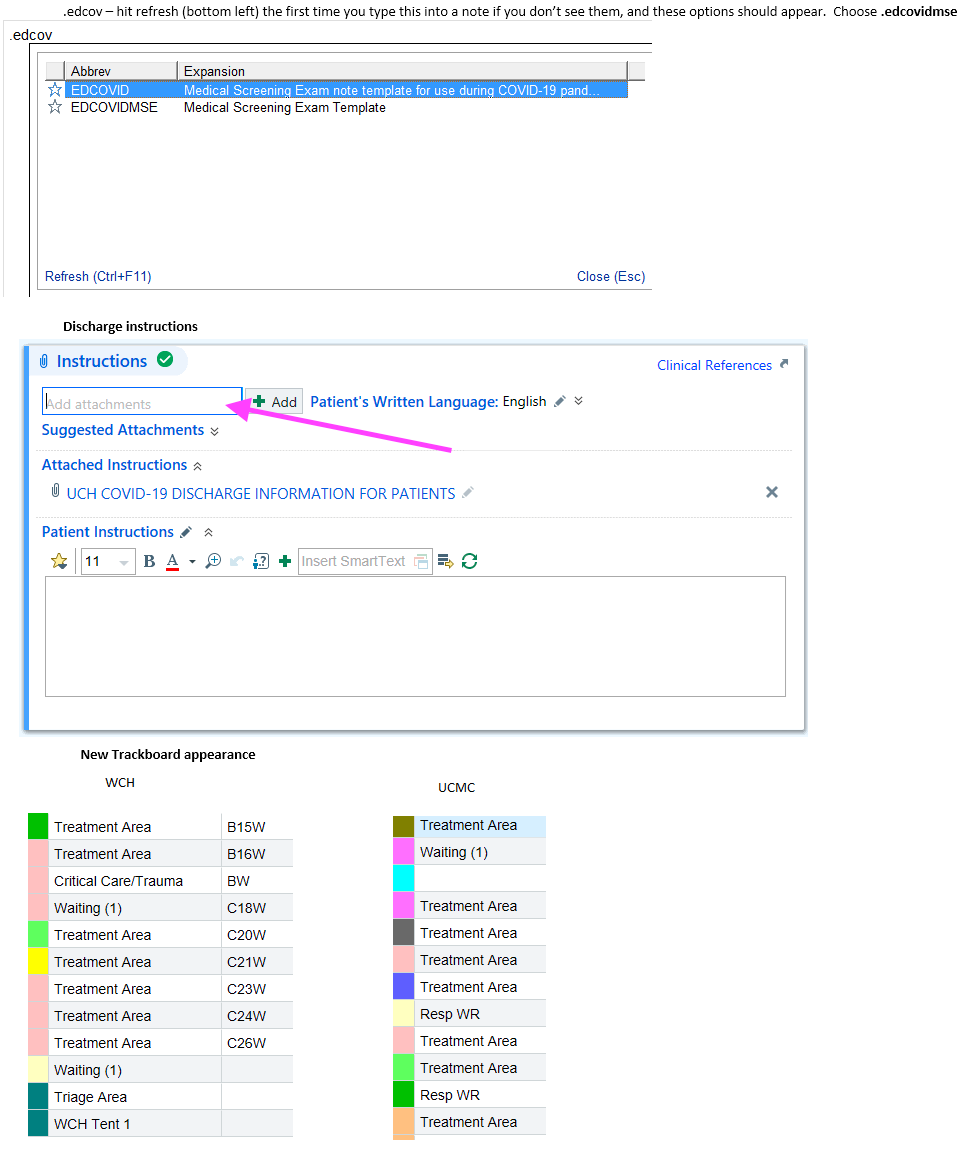
Medical Screening Exam (MSE) template – ATTENDINGS ONLY AT THIS TIME – for use in the respiratory ED’s and Tents.
- The note template is .edcovidmse. Type this in when you start a new note.
- This is an abbreviated chart template made specifically for patients who may have COVID
- There is a chance that you might not see the option the first time you type in .edcov. If that’s the case, hit the “refresh” option in the bottom left (see pic below). It should auto-populate from then on.
Discharge instructions – UC Health now has discharge instructions for COVID rule outs – use this option from here on instead of dotphrases
- See pic below – enter “COVID” into the discharge instructions box and the option should pull up. Thank you Dr. Kiser for providing and sharing temporary instructions with us to this point
Trackboard Changes - This is a work in progress, but temporarily, a column has been added to the left side of your screen to include patients in the tents, to differentiate them from the main waiting room.
- “Triage Destination” is the name of the column and reflects where they were originally placed.
- If they move to another area, “triage destination” remains the same.
- “Resp WR” = Tent at UCMC, “WCH Tent 1” = Tent at WCHSee pic below for WCH and UCMC screenshots.
- Again, a work in progress, and we will work to improve this but we wanted you to be aware of that change
Thank you and stay safe everyone,
Jack and Sanjay
Team,
Thank you again for the continued flexibility and patience with this ever dynamic COVID-19 situation. Things have been fairly mild at this point, but we are definitely starting to see some positives and sicker patients, though volumes remain low. I have attached our daily volume graphs for your continued awareness. Updates below:
1) Given low volumes anticipated for the next 1-2 weeks, we are going to try and get some people a break while we still can. Here is the deal:
- Attendings: If the volume is sufficiently low enough that the APod UH-3 attending feels comfortable managing the Main ED for the night, then it is reasonable to send the BPod attending home. This assessment should should take place around 1a-3a in the morning. This can/should only happen if the APod attending is comfortable doing so, and no questions asked if not. The CDU/Respiratory ED attending SHOULD stay through the night, as we are trying to limit movement back and forth between PODs while we still can. This also leaves a second attending in house in case there is an early morning volume surge.
- APPs: Please see the attached document built by the APP leadership and OPS team. The gist is that we will likely call off a morning APP if AM volumes are low, and shorten shifts in the afternoon/evening if volumes are low. Please be aware, we will still have appropriate APP coverage for MC, OBS, and the Respiratory ED during these times.
- Residents: For now, the lowest hanging fruit is sending the MC2 nighttime IPod resident home if volumes are low or if we close MC early. The OPS team and RLT are considering other options for nighttime down-staffing that are actively being considered and you will be updated shortly.
2) Cardiac arrests with COVID concerns:
- See the attached poster, which are printed and posted in outside of CDU 12 (and 11) and in the nurses station.
- If you are aware of an incoming cardiac arrest with COVID suspicion, the patient can be sent to CDU room 12, where we are set up to run arrests. Please see the attached poster for reminders about key features of COVID cardiac arrests, primarily related to appropriate PPE, minimizing staffing, utilizing the LUCAS, having a team to help outside the room, debriefing, and appropriate cleaning.
3) Surge planning
- For awareness, we have crafted plans for further surge that is anticipated for mid-April through May. When this is finalized in the coming days, I will make sure to share this with the group to know whats coming, and our triggers for each phase of expansion.
4) Trauma
- As Dr. Fermann mentioned in the WebEx, we are working with Trauma to improve both notification regarding COVID possible patients, as well as the best ways to evaluated patients both in the CDU/Respiratory ED and if/when we surge. More to come in the next few days.
5) Cardiology
- As most have seen on social, COVID is causing some impressively unorthodox STEMI/myocarditis presentations, leading to different protocols nationally. We are working with Cardiology actively to delineate their plans, which will likely involve the attached document from their society guidelines. However, there is still some ambiguity in this document, which I am pushing them to clarify (i.e. risk classification), and working with Pharmacy to ensure appropriate access to fibrinolytics, etc. Again, more to come on this.
- Big picture- call early, activate early. Ensure that if you are going to go to PCI that the teams are ready, and you can get the Interventionalist to the bedside to help determine the plan.
6) PPE
- This is literally changing every single day, so please ensure you are following Dr. Calhoun's emails closely. The ED is following their guidance on this, and will work to keep you up to date on any upcoming changes.
Thanks again, more to come in a few days.
Jack
Team,
A reminder that the new WCH ED attending schedule (announced a few months ago) will go into effect Wednesday, April 1 as below:
(Changes are in red and bolded)
| Weekdays | Non-military time |
| W1 0600-1400 (8 hours) W10 1000-1800 (8 hours) W2 1400-2200 (8 hours) W16 1600 - 0000 (8 hours) W18 1800-0200 (8 hours) W3 2200-0600 (8 hours) |
6a-2p 10a-6p 2p-10p 4p-12a 6p-2a 10p-6a |
| Weekends | |
| WCA 0600-1600 (10 hours) WC-10w 1000-2000 (10 hours) WC-15w 1500-2300 (8 hours) WC-16w 1600-0200 (10 hours) WCB 2000-0600 (10 hours) |
6a-4p 10a-8p 3p-11p 4p-2a 8p-6a |
|
As if you needed any more change in your lives right now. I appreciate everyone being understanding and flexible.
APP and resident schedules will remain the same at this time (morning APP still comes in at 7am) |
West Chester ED attendings,
Updates on a couple services and referrals to the WCH ED, where you may receive phone calls:
Psychiatry — referral calls
- Both Lindner and Beckett Springs have or are developing COVID-specific areas of care and can take care of patients in droplet/contact precautions
- Previously, calls went to our charge nurse from their nurses regarding patients being sent for a med eval
- In an effort to dampen the knee-jerk reflex to send COVID PUIs or confirmed cases to us who are otherwise medically stable, I’ve asked both facilities to utilize the capacity management center (584-BEDS) and speak to a WCH ED attending prior to transfer. My hopes are for a doc to doc conversation, but depending on time of day, it might be an RN to doc conversation.
- ***If you do get a call, please let them know we are more than happy to see anybody they feel needs evaluation; but you are welcome to help them understand our diagnostic and therapeutic processes for otherwise well COVID+ patients.***
- I realize that this will add some front-end work to your plates, but my goal is to ultimately offload your work as well as the strain on the system.
- Please let me know how/if this is working – I figured it was worth a try, but if it’s not working and slowing you down, then we’ll re-evaluate it
OB/GYN – Christ Liberty L&D Closed
- Christ Liberty has temporarily pulled their OBGYN from the L&D section of their campus
- They have worked out a protocol with Dr. Ian Foley (WCH OBGYN medical director) and Dr. Buckreus (prior medical director) for patients >20 weeks gestation to be evaluated in our L&D unit if they cannot go down to Christ Main
- The Chris Liberty ED is still open and will handle imminent deliveries, early pregnancy issues, and non-OB related >20 week pregnant patients
- You may get a call regarding a patient in labor (not imminent delivery) who’s coming our way, but we will continue to follow our triage criteria upon arrival, and if they are stable they will be taken directly to L&D without you knowing about their arrival.
- This shouldn’t impact us very much, but I wanted you to be aware because of at least two potential things you’ll be involved in.
- Fielding transfer calls (we don’t anticipate many, as all their patients know that they have temporarily closed their unit)
- In the case of a sudden change to a precipitous delivery in transfer
Thanks for your time, and I hope you’re all able to enjoy this beautiful day.
Sanjay
(617) 281-9416
Expand all
Collapse all
Contact Us
Department ofEmergency Medicine
Medical Sciences Building Room 1654
231 Albert Sabin Way
PO Box 670769
Cincinnati, OH 45267-0769
Mail Location: 0769
Phone: 513-558-5281
Email: roattw@ucmail.uc.edu